Body temperature is one of the most important objective indicators in the process of collecting medical history and data by clinical medical staff. Its accuracy and accuracy directly affect the diagnosis, treatment and care of the disease. In recent years, many scholars have carried out various researches on the equipment, methods, parts and time of body temperature measurement. In order to enable the nursing peers to further understand various temperature measurement methods, rationally select temperature measuring equipment to improve the accuracy of body temperature measurement, and provide reference and reference for the majority of nursing workers.
First, the choice of temperature measuring equipment
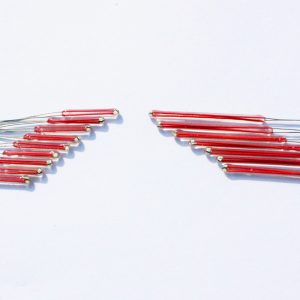
1. Contact temperature measuring equipment: mainly includes glass mercury thermometer, electronic thermometer and semiconductor thermometer. The mercury thermometer measures the temperature of the body by utilizing the physical properties of mercury in thermal expansion. Because mercury thermometers are cheap and stable in performance, they are the most widely used temperature measuring equipment in hospitals and homes in China. The electronic thermometer measures the temperature using the thermistor principle, and its measured body temperature is faster and more accurate than the mercury thermometer. The semiconductor thermometer uses a thermistor as a temperature sensing element to measure body temperature changes, and is often used to measure body temperature and skin temperature difference and to measure body temperature during low temperature anesthesia.
2, non-contact temperature measuring equipment: Tympanic thermometer is to indirectly obtain the temperature of brain tissue by measuring the infrared heat generated by the tympanic membrane and surrounding tissue. The infrared camera uses an uncooled focal plane infrared detector to display the infrared thermogram of the object in a pseudo-color image, thereby achieving the purpose of non-contact measurement of the surface temperature of the human body.
Second, temperature measurement parts and methods
1. Contact temperature measurement method
(1) Axillary temperature measurement method: Because the temperature measurement of the armpit is safe, convenient and easy for patients to accept, it is currently the most commonly used temperature measurement site in clinical practice. Its biggest advantage is its simplicity and continuous temperature measurement. The disadvantage is that the temperature measurement time is longer and the accuracy is not high. The temperature measurement time of the armpits is the same in all textbooks, all of which are 10 min, and many scholars study the difference between the temperature of the neck, back, abdomen, groin, elbow, rectum and other axillary temperature. Take 10 minutes as the standard. Chen Genzhi et al. compared the temperature measurement results of 5, 7 and 10 min under the armpit, and proposed 7 min as the optimum time for temperature measurement under the armpit. However, the randomized controlled trials conducted by Luo Ya et al. found that the temperature of the underarm was 5 min to achieve the purpose of accurately reflecting the patient’s body temperature. Foreign scholars believe that the temperature measurement time under the arm should be at least 3 minutes. The normal value of the armpit temperature is 36 ° C ~ 37.4 ° C. Precautions for temperature measurement of axillary fossa: a. When measuring temperature, the patient must close the upper arm to the thorax and seal the axillary fossa to form an artificial body cavity. b. The difference between normal armpit temperature and central temperature is 0.2 °C ~ 0.3 °C, and fever patients are 0.5 °C ~ 0.6 °C. Pay attention to this error when observing low fever patients. c. If the temperature of the ice pack is lowered, the influence time on the temperature of the ice is as long as 50 minutes. Therefore, the measurement of the temperature should not be carried out within 50 minutes after the ice pack is cooled. d. The bathing time of the patient who wiped the bath was 20 min, and the body temperature was measured after 30 min. e. For central hyperthermia venous cooling, the effect of venous cooling is strong, and the patient is also a central dysfunction of body temperature regulation, so the body temperature changes are measured after 15 minutes of cooling. f. Compared with the non-infusion side sputum temperature, the infusion side is significantly lower. Therefore, for patients who are on the upper limb infusion, the temperature should be measured on the opposite side. h. It is not suitable for patients with extreme weight loss because a closed artificial body cavity is required to ensure the accuracy of the temperature measurement result. j. When measuring the temperature, according to the book, the sweat should be dried under the armpits, and there should be no sweat in the armpits to avoid evaporation and heat dissipation, which affects the accuracy of temperature measurement. However, it has been reported in the literature that it is not necessary to dry the sweat, because a small amount of sweat passes through the 10 min clamp, and the sweat temperature is already close to the body surface temperature. Li Hejun also used the method of not drying dry sweat to observe and compare the anus temperature and temperature of neonates. The difference between the two was not significant. g. It should be kept long enough for the temperature measurement time, about 10 minutes, so that the deep temperature can be gradually transmitted and reach the dynamic balance. k. Differences in temperature between left and right sides: Yan Yun randomly selected 100 healthy adults to study bilateral temperature. The results showed that 87.0% of human body temperature was left high and right low, probably because the left side was more than the right side. Close to the large blood vessels. In general, measuring the temperature does not require distinguishing between the left and right sides, which may cause measurement errors. l. Upper limb hemiplegia: Lu Weiwei observed the temperature of the axillary fossa in 150 patients with cerebral vasospasm. The reason was that the temperature of the axillary fossa was significantly lower than that of the affected side. Increased local heat production, coupled with limb movement disorders, slow axillary heat dissipation, so the body temperature of patients with hemiplegia should be based on the healthy side. m. Upper limb fracture: Patients with fractures have extensive tissue damage on their affected side, tissue necrosis, inflammatory stimuli, etc., causing local tissue congestion and edema, which may lead to an increase in temperature. Liu Lanru et al. observed the temperature of the lower jaw of patients with upper extremity fractures and found that the affected side is generally higher than the healthy side. Therefore, when measuring the temperature of the upper limb fracture, the healthy side should be selected to reflect the temperature of the body. n. The amount of adipose tissue under the armpit: the heat conduction of human body fat is low, when the subcutaneous fat is more, the conduction heat from the deep to the surface layer is less, and the measured value is lower. Therefore, in patients undergoing breast cancer surgery in which axillary adipose tissue has been removed, the temperature of the affected side of the ankle is higher than that of the healthy side due to the axillary vein approaching the skin. p. Regularly check the thermometer to see if the thermometer is broken, the mercury column is not rising, or it cannot be below 35 °C.
(2) Oral temperature measurement method This method is still used in most countries of the world. Regardless of whether you use a mercury oral thermometer or an electronic oral thermometer, cross-infection can be basically avoided after strong disinfection. The advantage is that the operation is easy, painless, the temperature measurement value is less affected by the outside world, the sublingual temperature is slightly lower than the central temperature and the deep tissue temperature, and the difference is clinically negligible. The disadvantage is that continuous temperature measurement is not possible. Textbooks have different time requirements for oral temperature measurement, with 3 min, 3-5 min and 7-8 min. The results of self-control experiments conducted by Chen Genzhi and others showed that the oral temperature measurement time is preferably 5 min. For the area of oral temperature measurement, Shi Yan research found that it is better to put the thermometer under the tongue for 3 min, and the value measured on the tongue and the sublingual mouth is low. Precautions for oral temperature measurement: a. In addition to the effects of activities, diet, oral respiration, use of dental trays, oxygen and aerosol therapy, there are also some uncontrollable factors, such as too long time for patients to feel Fatigue requires high patient cooperation, so it is not suitable for children, mental disorders and unconscious patients. b. Immediately after eating or hot on the cheek, it should be measured after 30 minutes. c. If a patient accidentally bites a thermometer and swallows mercury, he or she should immediately take a large amount of liquid protein or milk to bind the protein to mercury to delay the absorption of mercury. It can also be given a large amount of leeks or swallowed in capsules to remove the mercury package.
(3) Intra-rectal temperature measurement is the only non-invasive invasive temperature measurement method. Because it is not affected by room temperature, there is a rich blood supply from the radial artery, which is often considered to be the most accurate and practical method outside the ICU. The body temperature in the ICU pulmonary artery catheterization center is the most accurate method. Due to the large trauma, this “gold standard” implementation is limited. However, studies comparing rectal temperature to pulmonary artery temperature suggest that rectal temperature lags behind changes in body temperature and is always higher than pulmonary artery temperature. Other disadvantages of rectal temperature measurement include the patient’s unwillingness to accept, occasional perforation, and the spread of intestinal pathogens or resistant flora. Despite this, most clinical studies still use rectal temperature as one of the important criteria for disease change. However, this method is limited by the patient’s body position and may cause paralysis in adults, so it is mostly used for body temperature monitoring in children. Some scholars have observed through experiments that as long as the depth of the thermometer inserted into the anus meets the requirements and is fixed, the measured values of the anus temperature at 1, 2, and 3 min are nearly the same, indicating that the anus temperature test can accurately reflect the true body temperature of the body within 1 min. Happening. The foreign rectal temperature measurement method is similar to that in China. The thermometer is inserted into the rectum 2~4 cm, the temperature is measured for 3 min or the thermometer is kept until the mercury is no longer raised for 2 min. The rectal temperature measurement matters: a. The patient in the shock phase should be used with caution because in shock During the period, the patient may have closed the blood flow from the rectum and produced the wrong measurement. b. Diarrhea, rectal or anal surgery, myocardial infarction patients should not be rectal temperature measurement. c. Those who take a bath or enema must wait 30 minutes before they can be tested.
(4) The sub-neck temperature measurement method allows the newborn to take the side or supine position, and use the disinfected spare anal table to store the mercury tank end (the mercury storage tank of the anus is thicker and shorter, which is safer than the slender mercury storage tank of the watch. Place it horizontally on the skin folds of the newborn’s neck and measure it for 3 minutes. Zhao Xia and others believe that the method is only suitable for children who are fatter than 1 year old. Because of its short neck and many wrinkles, it can clamp the thermometer, while the thinner or older children have neck. Relatively long, the skin of the neck cannot clamp the thermometer, which will affect the measurement results.
(5) The method of temperature measurement between the back and shoulders of the back is composed of the main branches of the radial artery. The blood supply is abundant, and the neonatal heat mainly depends on the decomposition of brown fat, while the brown fat is distributed around the large blood vessels and between the shoulder blades. The central warming system is formed in the area, armpits and neck. Zhang Xiaojing et al. showed that the measurement of the temperature between the back and shoulders of the newborn for 10 min can accurately reflect the body temperature of the newborn. Yan Xiaoying’s clinical observation of 100 patients with ICU back temperature also confirmed the feasibility of using back temperature measurement in bedridden patients. The method is to take the patient in the supine position, and insert the mercury storage tank end of the thermometer into the trapezius muscle part between the spine and the shoulder blade through the neck (left and right) (the back skin is closely attached to the underwear and the mattress), and the insertion length is 4.5. ~6.5 cm.
(6) Abdominal temperature measurement method The mercury part of the thermometer is placed at the left side of the umbilicus at 3 cm, and is fixed by the elastic band of the underwear. It is placed in a closed state and measured for 10 min. It is suitable for all age groups, especially suitable for inconvenient measurement of armpits and oral temperature. Such as coma, the elderly, extremely thin axillary emptiness and children.
(7) Inguinal temperature measurement method for infants and young children, some scholars put the thermometer head in the groin and the internal junction (ie, the femoral artery pulsation) to observe the inguinal temperature measurement, the results suggest that infants under 3 years old use the groin Temperature instead of measuring the temperature is completely feasible. The inguinal temperature measurement method is also suitable for large-area burns in other parts.
(8) Elbow nest temperature measurement method The mercury end of the thermometer is placed in the elbow of the patient, the upper arm is adducted and the forearm is bent upwards (the finger can be placed on the shoulder) and the thermometer is clamped for 10 minutes. Hu Rong obtained a clinically unsatisfactory result of the temperature measured in the elbow fossa and armpit. This method provides a simple and easy new test for patients who are not suitable for other temperature measurement sites. Warm part. In addition, because in the summer, the armpits are sweaty, and the sweat in the elbows evaporates quickly. There is no need to wipe the sweat when measuring the temperature. Therefore, in the special case of the hot season, the temperature of the armpit can be replaced by the temperature of the armpit.
(9) Hand temperature measurement The patient’s index finger, middle finger, ring finger and little finger’s finger pad and palm hold the mercury end of the thermometer for 10 min. As long as the patient’s palm has no scars, the person can clench his fist. Some scholars have observed the diurnal variation of normal human hand temperature (ie, peripheral limb temperature) and the variation range of different individual hand temperature, and found that the normal human hand temperature ranged from 33.94 ° C to 37.28 ° C.
(10) Nasal temperature measurement can be performed using a common sputum table. The head of the watch is coated with a thin grease and gently inserted into the nasal cavity until it comes into contact with the inner wall of the nasal cavity. The temperature of this part can indirectly reflect the central temperature. Because of the influence of breathing, it is not as accurate as the tympanic membrane. Mainly used for monitoring during general anesthesia, but patients who are deprived of oxygen cannot use it.
(11) Bladder and urine temperature measurement For patients who need to keep the catheter, a catheter with a temperature probe can be used. The new probe is the temperature value of the radio wave transmission. The temperature of the part is the local temperature of the bladder, and the temperature is very close to the central temperature. It is suitable for the urinary system with inflammation, postoperative monitoring and critical patient observation. Units that lack equipment can use urine to measure temperature. At room temperature of 20 ° C, the temperature of 100 ml of urine in a plastic container is measured immediately. The obtained value and the temperature measurement in the bladder are only 0.1 ° C, which is more accurate than oral temperature measurement and is worthy of promotion. Nierman et al compared the bladder temperature to the tympanic membrane and pulmonary artery temperature. After 32 h of study, the deviation from the lung temperature record was 0.04 °C. The difference between the core temperature and the variable temperature was considered to be significant at ±0.2 °C. Therefore, the results of this study suggest that the bladder temperature accurately represents the “core temperature.” However, Kleeman et al. believe that bladder temperature may limit application because it is affected by a decrease in urine production, which means that it is limited in monitoring critically ill patients. At the same time, like the rectum, the bladder has no temperature receptors and is far from the hypothalamus, so the application of this method does not seem to be extensive enough.
(12) Vaginal temperature measurement The general temperature table is used, but strict disinfection is required. This part can accurately reflect the pelvic temperature and deep tissue temperature. The experiment found that when the infection occurred in this part, there was a local temperature increase.
2. Non-contact body surface temperature measurement
(1) External auditory canal (tympanic membrane) temperature measurement method Because the tympanic membrane and surrounding tissues are close to the hypothalamic body temperature regulation center, and the lower tympanic membrane and hypothalamus are supplied by the internal carotid artery, the infrared ear thermometer can obtain better body temperature by external ear canal temperature measurement method. It represents the deep temperature of the body and is widely used abroad. It is the first choice for children, parents and nurses. The tympanic membrane temperature measurement method is suitable for departments that need rapid non-invasive body temperature measurement, such as emergency room, “atypical pneumonia”, and large-area burn patients, but it is not suitable for departments that need to accurately measure body temperature. The Fisk study found that there was a large difference between the tympanic membrane temperature and the pulmonary artery catheter temperature, with a difference of >1.11 °C, which led to a 4% misdiagnosis rate. The measurement is required to be high. The patient should be aligned with the opposite side of the patient. Insert the thermometer probe into one ear canal, gently move the probe to the horizontal position, and then observe the temperature detection window. Read the measured value when the body temperature number no longer increases.
(2) Infrared thermal imager temperature measurement The use of infrared thermal imager for the initial screening of the body temperature of the population has played a significant role during the SARS epidemic in China. When measuring, ensure that the detection distance is 3~5 m, and the front of the subject can be aligned with the lens for 1 s. However, Zhang Yuanchao and others believe that although it has the advantages of high degree of automation, quick and convenient operation, and reduced chance of cross-infection, its measured temperature is lower than the mouth temperature by 1.40 ° C to 2.16 ° C, which cannot replace the mercury thermometer for clinical use. Similarly, foreign scholars also believe that the body temperature measured by this method exceeds 35.6 °C, which may indicate fever, so it is only suitable for the screening of fever patients in a large number of people entering and leaving the airport, such as airports, stations, and traffic routes.
Body temperature measurement is one of the important indicators for medical staff to perform physical examination, diagnosis of diseases and vital signs monitoring for patients or healthy people. It is also one of the most basic nursing contents in nursing work, and its accuracy directly affects the diagnosis and treatment of diseases. And care. Regarding the research of body temperature measurement, many scholars at home and abroad have carried out a lot of researches on temperature measuring equipment, temperature measuring parts, temperature measuring methods and temperature measuring time, and summarized many useful experiences and insights. However, comparative studies on the standardized measurement of body temperature and non-standardized measurement of body temperature by nursing staff are rarely reported. Thus,In the future work, nursing peers should pay attention to strengthen research on this aspect, so that the most basic nursing operation technology of body temperature measurement can be more standardized and scientific, improve the quality of care, and better serve patients.